How to Tell That You Have a Gastric Leak
Agastric sleeve leak is a rare but serious complication that can occur after bariatric surgery. While gastric sleeve procedures are highly effective for long-term weight loss, leaks along the staple line can disrupt recovery if not identified early. Knowing the symptoms of gastric sleeve leak and recognizing when to seek medical help is essential for protecting your health and ensuring proper healing after surgery.
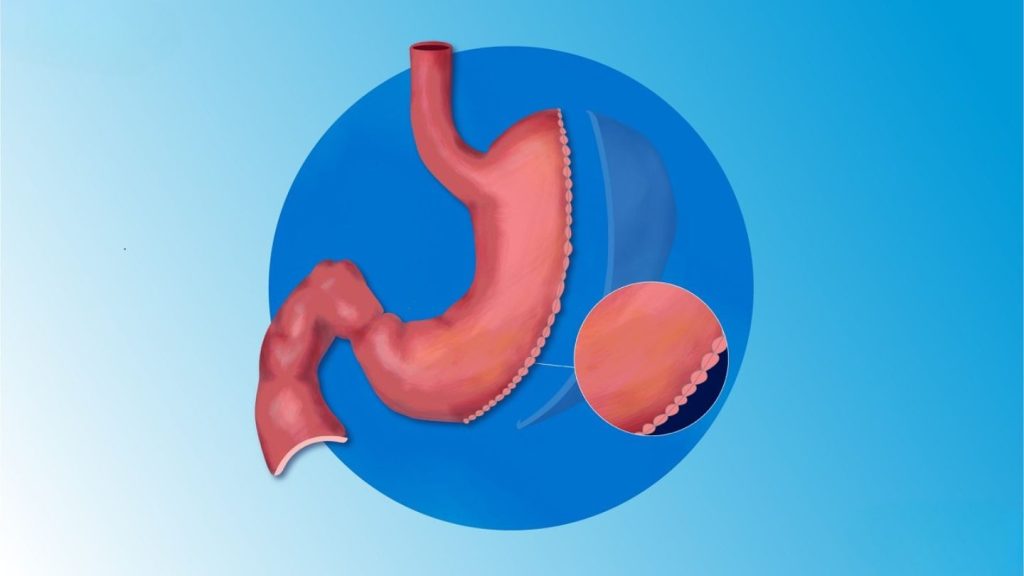
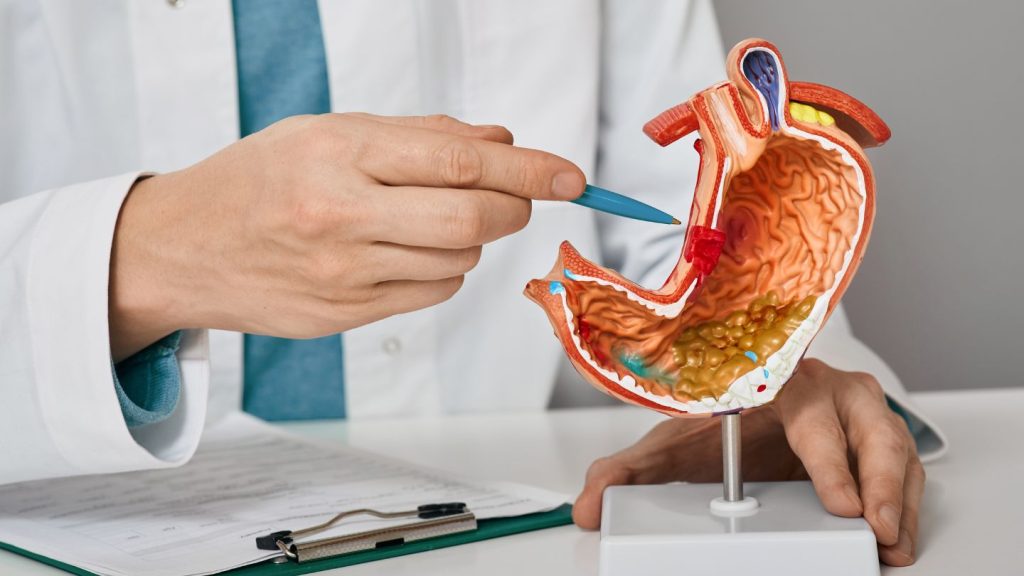
What Is a Gastric Sleeve Leak?
A gastric sleeve leak occurs when the new stomach pouch, created during bariatric surgery, develops an opening or separation along the staple line. This allows stomach contents, such as fluids, food, and digestive enzymes, to escape into the abdominal cavity. When this happens, it can trigger inflammation or infection, requiring immediate medical attention.
Although this condition is uncommon, patients should understand how to know if you have a leak after gastric sleeve to respond quickly. Leaks can appear within days after surgery (known as early leaks) or develop weeks later (late leaks). The risk may increase with factors like infection, poor wound healing, or excessive strain on the surgical site.
Early Warning Signs of a Gastric Sleeve Leak
Recognizing the signs of gastric sleeve leak early can be lifesaving. The body usually gives several warning indicators that should never be ignored. Some of the most common gastric leak symptoms include:
- Persistent or severe abdominal pain that worsens over time
- Fever or chills that indicate infection
- Rapid heart rate (tachycardia), typically over 120 beats per minute
- Nausea or vomiting that doesn’t improve
- Shoulder or chest pain caused by trapped gas or irritation of the diaphragm
- Fatigue or dizziness
While these signs can resemble normal post-operative discomfort, prolonged or worsening symptoms often signal an underlying problem. Postoperative discomfort and fatigue are common during the initial recovery period, but understanding how to manage these effects can make recovery smoother. Learning seven tips to feel better during gastric sleeve surgery recovery can help patients distinguish normal healing responses from symptoms that need medical attention. Patients frequently ask, “how do you know if your gastric sleeve is leaking?” The best answer is to trust your instincts; if something feels off, contact your surgical team immediately. Early detection allows for faster treatment and reduces the risk of serious complications.
Read More: Signs You Might Need Bariatric Revision Surgery
How Doctors Diagnose Gastric Sleeve Leaks

When a leak is suspected, physicians perform several tests to confirm the diagnosis. Imaging studies, such as a CT scan or an upper GI contrast study, can pinpoint where fluid is escaping from the stomach. Blood tests are also used to detect infection or inflammation. Once identified, the care team determines whether the leak can be managed non-surgically or requires immediate intervention.
Knowing the signs of leak after gastric sleeve helps ensure that patients don’t delay seeking care. Even mild discomfort can escalate if the underlying cause is a staple line leak. Digestive complications can also mimic symptoms of leaks, making an accurate diagnosis essential. For instance, issues like moderate and severe constipation after a gastric sleeve can cause abdominal pressure and discomfort, underscoring the need for a clear medical evaluation before assuming a leak.
Common Causes of Gastric Sleeve Leaks
Leaks can develop for a variety of reasons. Some of the most common causes include:
- Surgical factors: High pressure along the staple line or improper closure can weaken the area.
- Tissue ischemia: Poor blood flow to the staple line may delay healing.
- Infection or inflammation: These conditions can erode tissue integrity.
- Post-surgical strain: Eating solid foods too soon or not following postoperative dietary guidelines can stress the stomach pouch.
Lifestyle factors such as carbonated beverages can also impact recovery. Patients often wonder whether options like Coke Zero after a gastric sleeve are safe, highlighting the importance of moderation and surgeon-approved dietary habits during healing. Adhering to your surgeon’s recovery instructions reduces these risks. Maintaining proper hydration, avoiding large meals, and attending follow-up appointments are crucial to preventing complications.
Read More: Can You Have Carbonated Drinks After Bariatric Surgery?
What Happens If You Have a Leak After Gastric Sleeve
Patients often wonder, “what happens if you have a leak after gastric sleeve?” The answer depends on the leak’s severity and timing. Minor leaks may be treated with antibiotics, drainage, and nutritional support, while larger leaks often require endoscopic or surgical repair.
During recovery, your doctor may recommend temporary fasting or tube feeding to allow the stomach time to heal. In some cases, stents are placed inside the stomach to seal the leak and promote tissue closure. With prompt medical attention, most leaks can be successfully managed, leading to full recovery.
How to Prevent a Gastric Sleeve Leak
Prevention begins with preparation and post-operative discipline. Here are strategies that reduce your risk of developing gastric sleeve leak symptoms:
- Follow dietary stages carefully: Gradually progress from clear liquids to pureed foods before reintroducing solids.
- Avoid overexertion: Heavy lifting or intense exercise too soon can increase abdominal pressure.
- Maintain protein and nutrient intake: Adequate nutrition supports tissue repair and overall healing.
- Stay in close contact with your bariatric team: Regular checkups allow professionals to monitor progress and detect complications early.
Consistent postoperative monitoring plays a major role in preventing complications and supporting recovery. Understanding the importance of follow-up after gastric sleeve care surgery emphasizes why scheduled visits are essential for identifying potential issues like leaks, nutritional deficiencies, or slow healing before they progress. These preventive habits not only protect against leaks but also promote successful long-term weight management.
Recovery and Long-Term Outlook

Most patients who experience a gastric leak recover completely with proper care. Once the leak is repaired and the infection clears, the focus shifts to rebuilding strength and reestablishing healthy eating patterns. Patients are advised to monitor any recurring gastric leak symptoms and report them immediately. Even months after surgery, new discomfort should be evaluated to rule out late leaks or scar-related complications.
Developing awareness about signs of leak after gastric sleeve empowers patients to act decisively. The earlier the issue is addressed, the faster the healing process and the lower the risk of severe infection.
Read More: Signs You Might Need Bariatric Revision Surgery
Final Thoughts on Recognizing a Gastric Sleeve Leak
Understanding the symptoms of gastric sleeve leak is crucial for every patient recovering from bariatric surgery. Early detection, clear communication with your surgeon, and adherence to recovery protocols can prevent complications and ensure smoother healing.
If you ever notice unusual pain, fever, or digestive distress after surgery, don’t wait for it to worsen; seek medical attention immediately. Awareness and swift response remain your best defenses against serious post-operative complications.
At the Lenox Hill Bariatric Surgery Program, our team, specializing in bariatric surgery in New York, provides advanced postoperative monitoring, nutritional counseling, and complication management to ensure patient safety at every step. We help patients recognize potential warning signs, manage recovery effectively, and achieve long-term success after gastric sleeve surgery in New York.
Frequently Asked Questions
What are the first signs of a gastric sleeve leak?
The most common early symptoms include sharp abdominal pain, rapid heart rate, fever, and nausea. If these persist beyond normal recovery discomfort, contact your healthcare provider immediately.
How soon after surgery can a gastric sleeve leak occur?
Leaks can appear within a few days to several weeks after surgery. Early leaks are more common, but late leaks may develop if tissue healing is delayed.
Can a gastric sleeve leak heal on its own?
Minor leaks may close naturally with proper rest, antibiotics, and nutrition support. However, most cases require medical supervision or endoscopic intervention to ensure complete healing.
What causes a gastric sleeve to leak?
The main causes include staple line tension, poor blood flow, or infection. Eating solid foods too early or ignoring postoperative guidelines can also increase the risk.
How can I reduce my risk of developing a gastric leak?
Follow your surgeon’s dietary instructions, avoid heavy lifting, and attend all follow-up appointments. Prioritizing rest, hydration, and nutrient-rich foods helps promote healing and prevent complications.